Welcome to the OMA Blog
The Obesity Medicine Association Blog is the leading industry hub for obesity medicine. Find the latest research, expert insights, and practical tips to tackle the multifaceted disease of obesity. Hear from OMA Outreach Committee members, OMA Board members, and more to gain a deeper understanding of the complex factors influencing obesity and explore innovative approaches to prevention, treatment, and long-term management. Join a community of healthcare professionals, researchers, and individuals passionate about combating obesity.
View by Category

Obesity and Insulin Resistance: Symptoms, Diagnosis, and Treatment
Explore the link between obesity and insulin resistance. Understand the risk factors, symptoms, and treatments for this dual health challenge.

New “Supportive Obesity Care” Website for Healthcare Professionals
Our society can be hostile toward people with obesity who commonly face judgment, prejudice, and unfair treatment in their daily lives. This problem extends to the healthcare setting, where patients can face weight bias and stigma from physicians, nurses, psychologists, dietitians, medical students, and even healthcare professionals who specialize in obesity.

Insulin and Weight Gain: Understanding the Connection
Insulin is a commonly used medication to treat patients with both type 1 and type 2 diabetes. Weight gain is a commonly seen side effect. Patients may have questions about insulin and potential weight gain out of concern for their appearance or their health (or both).

Is BMI Outdated? An Analysis of Body Mass Index and Health
Does your health care provider talk to you about your Body Mass Index (BMI) and do you know what it really means? Widely criticized as…

Obesity and Genetics: What is the Connection?
Is obesity genetic? Do our genes determine if we'll have a healthy body weight or not? Explore the role of genetics in the obesity epidemic.

The Obesity Paradox Explained: Is It Still Valid?
The "obesity paradox" suggests that individuals with overweight or obesity may have lower mortality rates in certain conditions. However, recent research challenges this.
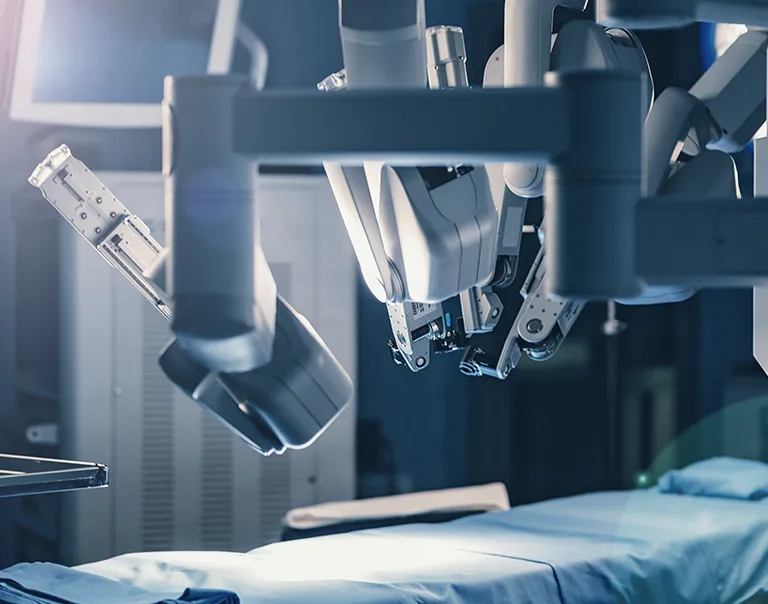
Bariatric Surgery Candidates: Who Meets the Requirements?
Bariatric surgery has emerged as a transformative option for individuals with obesity who are struggling to lose weight from other forms of obesity treatment. However,…

Obesity and Life Expectancy Trends in the U.S.
This article explores the relationship between obesity and declining life expectancy in the U.S.

Obesity and Heart Disease: Risks, Treatments, and Outcomes
Obesity and heart disease share a complicated relationship, and some of the same drugs may have effects on both obesity and cardiovascular health.
